To fully understand this post, please read Part One of the series on Genetics and Illness.
Early in my career, while taking a family medical history, I listened for incidences of family illnesses to help discern whether the child’s issue was an isolated case or could be due to genetics. Now I know how to look beyond genetics for further insights by identifying inflammation from food and other sources.
Case: celiac symptoms without celiac disease
Here’s a case from my own life. At the age of forty, I discovered I had a gluten sensitivity—as do both of my sisters, both of my parents, and one of my nieces. None of us meet the medical diagnostic criteria for celiac disease, but we all had health issues that either resolved completely or improved significantly when we stopped eating gluten. Here’s a list of our gluten-related complaints:
- Constipation
- Hemorrhoids
- Stomach pain, bloating, excess gas
- Weight gain
- Brain fog
- Joint pain
- Rosacea (red rash on the cheeks)
- Anemia
- Lack of energy
This certainly sounds like something with a genetic basis, doesn’t it?

Gluten and My Family’s Genetic History
Assessing a family medical history includes distant heritage and ethnic tendencies toward certain diseases, which can also provide significant information. As I mentioned in Part One, celiac disease is more prevalent in people of Northern European descent, specifically Irish, Scottish, and English. I have Irish, Scotch, and German roots, so I need to pay attention to my symptoms, my family’s history, and my ethnic background.
The discussion about gluten and my family always reminds me of my beloved paternal grandmother, Vonnie. She had stomach issues and ulcers her entire life and ended up dying with lymphoma. Individuals with undiagnosed celiac disease who continue to eat gluten have a three times higher rate of lymphoma than the general population. I now suspect that she may have had celiac disease, or possibly what the rest of us have, but she was just never diagnosed with it. The good news, however, is that once you go off gluten and your gut heals, your risk of lymphoma decreases to the same rate as that of the general population.
Antibody-Negative Gluten Sensitivity or Celiac?
Dr. William Davis, a cardiologist who wrote the book Wheat Belly, would describe what my family members and I have as antibody-negative gluten sensitivity. We have many celiac disease symptoms, but our bodies don’t make the classic antibody we test for in conventional laboratory tests. Stay tuned to the blog for more about food testing.

I share with you my own family’s history because we are a good example of how important it is to understand the subtle differences between food allergies, food sensitivities, food intolerance, and celiac disease. If I had relied solely upon a conventionally trained medical doctor, they would have told me I didn’t need to be off gluten because I didn’t have a true allergy to wheat gluten. And if I’d started eating it again, my symptoms would have come flooding back, and I would have ended up with a diagnosis of fibromyalgia or chronic fatigue syndrome.
Celiac and the Autoimmune Process
Celiac disease involves an Autoimmune (AI) process where the body (in particular, the lining of the GI tract) creates an immune response to the gluten molecule (a protein found in wheat, barley, rye, and many other processed foods). Gut inflammation ensues, leading to a host of symptoms in the GI tract, and elsewhere in the body. One 2001 Italian study showed that thyroid disease is three times higher in patients with celiac disease. The good news, however, is that when these patients go off gluten, a significant number of them experience resolution of their thyroid disease. Coming out of my medical residency the concept that any AI condition might be reversed was, for all practical purposes, blasphemy to my conventionally trained mind. I had learned that AI diseases are lifelong and progress until there is so much tissue damage that the original tissue no longer functions.
When I first started practicing medicine in 2002, AI conditions in kids were rare. However, over the past 30 years, the global prevalence has increased significantly. Currently, 5 percent of the pediatric population has an AI illness, with Autoimmune Thyroid Disorders (AITD) being the most common. The prevalence of AITD among kids with celiac disease ranges anywhere from 2 percent, to as high as 40 percent. In conventional pediatrics, if a child has constipation or AITD, we may test them for celiac disease (IgA antibodies) and for allergies to dairy and wheat (IgE antibodies). If those are negative, we advise the child to continue eating those foods.
Food Sensitivities and Celiac
This is why understanding food sensitivities is essential. The children with negative tests for allergies and celiac disease may still have sensitivities to these foods, and if so, consuming these foods will cause excessive systemic inflammation. This was my case with gluten and dairy — I was not allergic to either, and did not have celiac disease, but eating them was throwing everything out of whack.
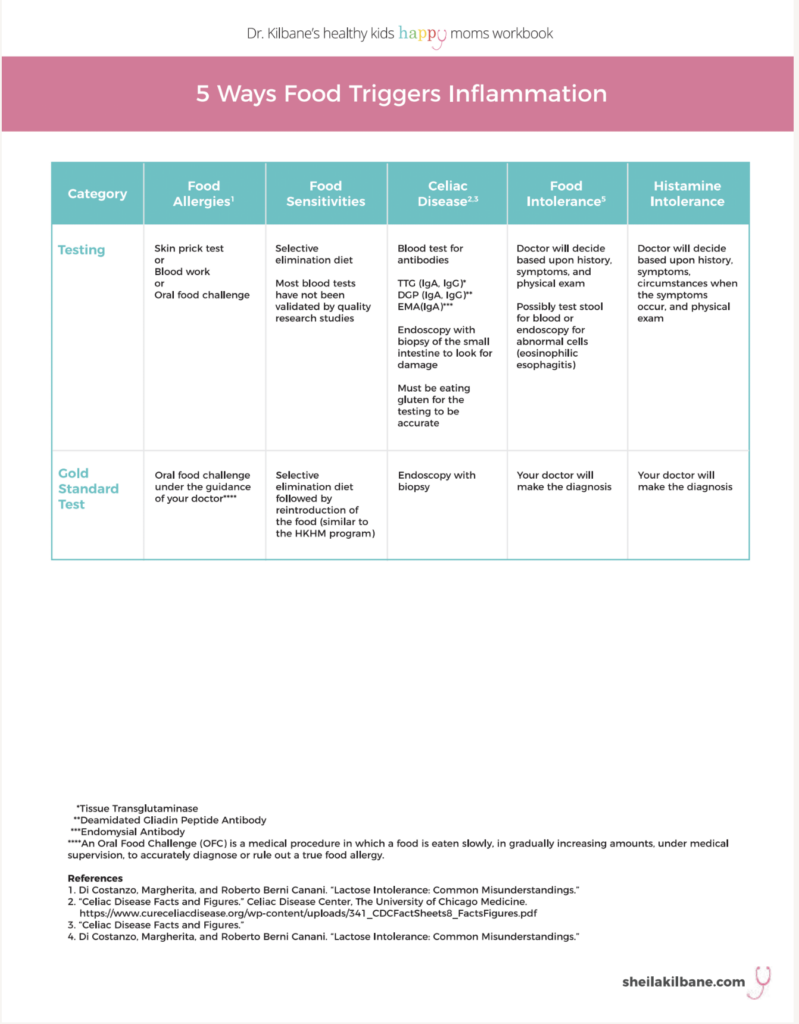
Food sensitivities are best assessed by doing a selective elimination diet. Blood tests which look for food sensitivities (IgG antibodies) have become more and more popular, but from conventional medicine’s standpoint, they are controversial. I use them in certain situations in my practice, but as of the writing of this blog, I most often use a selective elimination diet to determine food sensitivities.
This video is part of my online course. It explains that celiac disease is an autoimmune condition and how it can be detected; the difference between allergies, sensitivities and celiac; why an elimination diet is the Gold Standard for identifying inflammatory foods.
Where and How to Begin Understanding Food Reactions
The complexity of testing for food reactions led me to write an entire chapter on the topic, in my book. If I had not figured out the connection between gluten, dairy, and my health, and if I had continued to eat them, I most certainly would not have felt good enough to continue practicing medicine!
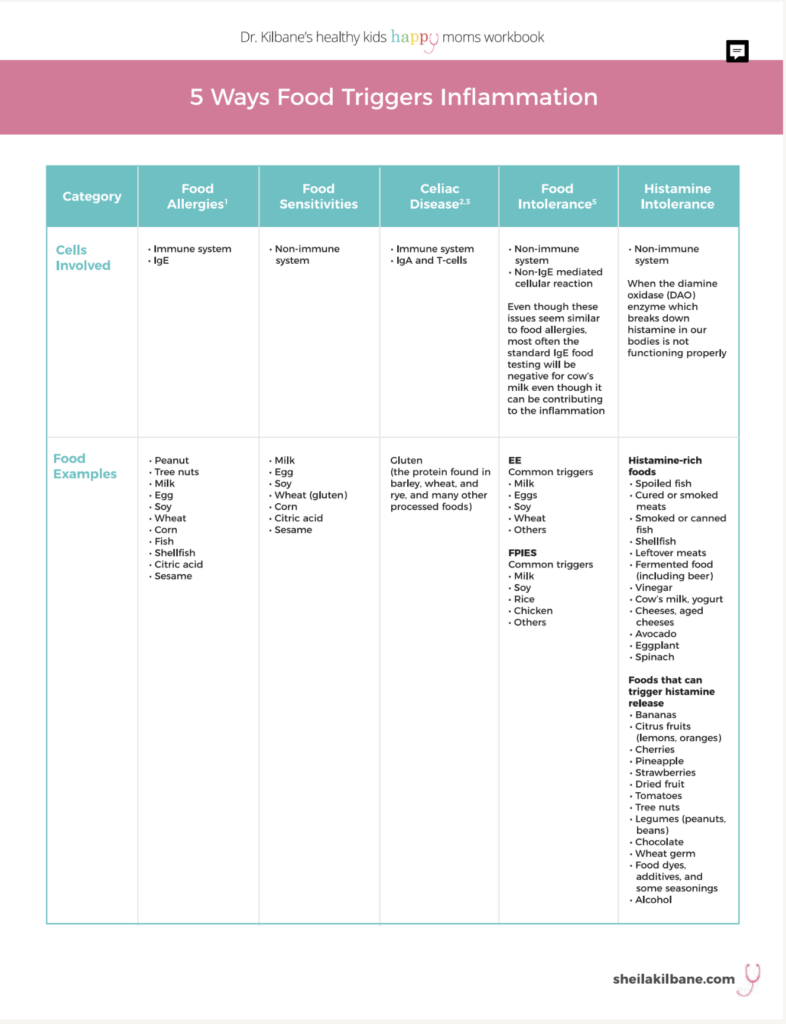
I created a three-page table on food and inflammation for my Healthy Kids, Happy Moms Workbook. Some of what you find may surprise you!
Because of my personal experience and my integrative medical training, the way I interpret the family history now is very different from the way I did 15 years ago. Conventional medicine systems and integrative medicine systems view family history through different lenses. Conventional medicine trains doctors to look for the diagnosis and treat it with medications and/or surgery. In integrative medicine, we are trained to look for patterns and view all symptoms as related, aiming to uncover the underlying cause of the inflammation.
Here’s an easy way to begin lowering systemic inflammation, take my free one-week Mini-Cleanse, which is just one part of my online course that supports my book and workbook.
If you are interested in a 15 minute consult on your child’s health, visit my private practice website.
Takeaways
- There are subtle differences between food allergies, food sensitivities, food intolerance, and celiac disease.
- Celiac disease is different from antibody-negative gluten sensitivity, meaning the patient has tested negative for celiac disease but they become symptomatic when eating gluten.
- Celiac disease involves an Autoimmune (AI) process.
- The prevalence of Autoimmune Thyroid Disorders (AITD) among kids with celiac disease ranges anywhere from 2 percent, to as high as 40 percent.
- The children with negative tests for food allergies and celiac disease may still have sensitivities to these foods, and if so, consuming these foods will trigger systemic inflammation.
- Food sensitivities are best assessed with a selective elimination diet.
- Integrative medicine is a powerful combination of conventional medicine partnered with natural and nutritional therapies. The blend of both systems taps into the body’s innate healing capabilities.
Armed with the right information, guidance, and structure, the nutrition and supplement recommendations in the Healthy Kids, Happy Moms program are doable, clear, and offer the possibility of changing your child’s health forever.